Lactate dehydrogenase
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||
Lactate dehydrogenase (LDH or LD) is an enzyme (EC 1.1.1.27) present in a wide variety of organisms, including plants and animals.
Lactate dehydrogenases exist in four distinct enzyme classes. Two of them are cytochrome c-dependent enzymes with each acting on either D-lactate (EC 1.1.2.4) or L-lactate (EC 1.1.2.3). The other two are NAD(P)-dependent enzymes with each acting on either D-lactate (EC 1.1.1.28) or L-lactate (EC 1.1.1.27). This article is about the NAD(P)-dependent L-lactate dehydrogenase.
Contents |
Reactions
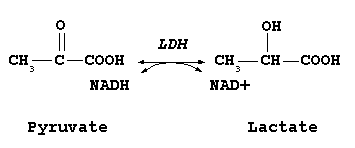
Lactate dehydrogenase catalyzes the interconversion of pyruvate and lactate with concomitant interconversion of NADH and NAD+. It converts pyruvate, the final product of glycolysis to lactate when oxygen is absent or in short supply, and it performs the reverse reaction during the Cori cycle in the liver. At high concentrations of lactate, the enzyme exhibits feedback inhibition and the rate of conversion of pyruvate to lactate is decreased.
It also catalyzes the dehydrogenation of 2-Hydroxybutyrate, but it is a much poorer substrate than lactate. There is little to no activity with beta-hydroxybutyrate.
Enzyme isoforms
Functional lactate dehydrogenase are homo or hetero tetramers composed of M and H protein subunits encoded by the LDHA and LDHB genes respectively:
- LDH-1 (4H) - in the heart and RBCs
- LDH-2 (3H1M) - in the reticuloendothelial system
- LDH-3 (2H2M) - in the lungs
- LDH-4 (1H3M) - in the kidneys, placenta and pancrease
- LDH-5 (4M) - in the liver and striated muscle
The five isozymes that are usually described in the literature each contain four subunits. The major isozymes of skeletal muscle and liver, M4, has four muscle (M) subunits; while H4 is the main isozymes for heart muscle in most species, containing four heart (H) subunits. The other variants contain both types of subunits.
Usually LDH-2 is the predominant form in the serum. A LDH-1 level higher than the LDH-2 level (a "flipped pattern"), suggests myocardial infarction (damage to heart tissues releases heart LDH, which is rich in LDH-1, into the bloodstream). The use of this phenomenon to diagnose infarction has been largely superseded by the use of Troponin I or T measurement.
Genetics in Humans
The M and H subunits are encoded by two different genes:
- The M subunit is encoded by LDHA, located on chromosome 11p15.4 (Online 'Mendelian Inheritance in Man' (OMIM) 150000)
- The H subunit is encoded by LDHB, located on chromosome 12p12.2-p12.1 (Online 'Mendelian Inheritance in Man' (OMIM) 150100)
- A third isoform, LDHC or LDHX, is expressed only in the testis (Online 'Mendelian Inheritance in Man' (OMIM) 150150); its gene is likely a duplicate of LDHA and is also located on the eleventh chromosome (11p15.5-p15.3)
Mutations of the M subunit have been linked to the rare disease exertional myoglobinuria (see OMIM article), and mutations of the H subunit have been described but do not appear to lead to disease.
Medical use
Tissue breakdown elevates levels of LDH, and therefore a measure of it indicates, e.g., hemolysis. Other disorders indicated by elevated LDH include cancer, meningitis, encephalitis, acute pancreatitis, and HIV.
Hemolysis
In medicine, LDH is often used as a marker of tissue breakdown as LDH is abundant in red blood cells and can function as a marker for hemolysis. A blood sample that has been handled incorrectly can show false-positively high levels of LDH due to erythrocyte damage.
It can also be used as a marker of myocardial infarction. Following a myocardial infarction, levels of LDH peak at 3-4 days and remain elevated for up to 10 days. In this way, elevated levels of LDH (where the level of LDH1 is higher than that of LDH2) can be useful for determining if a patient has had a myocardial infarction if they come to doctors several days after an episode of chest pain.
Tissue turnover
Other uses are assessment of tissue breakdown in general; this is possible when there are no other indicators of hemolysis. It is used to follow-up cancer (especially lymphoma) patients, as cancer cells have a high rate of turnover with destroyed cells leading to an elevated LDH activity.
Exudates and transudates
Measuring LDH in fluid aspirated from a pleural effusion (or pericardial effusion) can help in the distinction between exudates (actively secreted fluid, e.g. due to inflammation) or transudates (passively secreted fluid, due to a high hydrostatic pressure or a low oncotic pressure). The usual criterion is that a ratio of fluid LDH versus upper limit of normal serum LDH of more than 0.6[1] or ⅔[2] indicates an exudate, while a ratio of less indicates an exudate. Different laboratories have different values for the upper limit of serum LDH, but examples include 200[3] and 300[3] IU/l[4]. In empyema, the LDH levels, in general, will exceed 1000 U/l.
Meningitis and encephalitis
The enzyme is also found in cerebrospinal fluid where high levels of lactate dehydrogenase in cerebrospinal fluid are often associated with bacterial meningitis. High levels of the enzyme can also be found in cases of viral meningitis, in general indicating the presence of encephalitis and poor prognosis.
HIV
LDH is often measured in HIV patients as a non-specific marker for pneumonia due to Pneumocystis jiroveci (PCP). Elevated LDH in the setting of upper respiratory symptoms in an HIV patient suggests, but is not diagnostic for, PCP. However, in HIV-positive patients with respiratory symptoms, a very high LDH level (>600 IU/L) indicated histoplasmosis (9.33 more likely) in a study of 120 PCP and 30 histoplasmosis patients.[5]
Dysgerminoma
Elevated LDH is often the first clinical sign of a dysgerminoma. Not all dysgerminomas produce LDH, and this is often a non-specific finding.
See also
- Oxidoreductase
- Dehydrogenase
References
- ↑ Heffner J, Brown L, Barbieri C (1997). "Diagnostic value of tests that discriminate between exudative and transudative pleural effusions. Primary Study Investigators". Chest 111 (4): 970–80. doi:10.1378/chest.111.4.970. PMID 9106577.
- ↑ Light R, Macgregor M, Luchsinger P, Ball W (1972). "Pleural effusions: the diagnostic separation of transudates and exudates". Ann Intern Med 77 (4): 507–13. PMID 4642731.
- ↑ 3.0 3.1 Joseph J, Badrinath P, Basran GS, Sahn SA (November 2001). "Is the pleural fluid transudate or exudate? A revisit of the diagnostic criteria". Thorax 56 (11): 867–70. PMID 11641512. PMC 1745948. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1745948/pdf/v056p00867.pdf.
- ↑ doi:10.1186/1471-2466-2-1
This citation will be automatically completed in the next few minutes. You can jump the queue or expand by hand [1] - ↑ Butt AA, Michaels S, Greer D, Clark R, Kissinger P, Martin DH (July 2002). "Serum LDH level as a clue to the diagnosis of histoplasmosis". AIDS Read 12 (7): 317–21. PMID 12161854.
|
|||||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
_1I10.png)